2 Patterson Jr Grabois M Locked-in Syndrome a Review of 139 Cases Stroke 198617(4)758
This article has been cited by other articles in ScienceCentral.
Abstract
Locked-in Syndrome is a severe pontine stroke causing quadriplegia, lower cranial nerve paralysis, and mutism with preservation of only vertical gaze and upper eyelid movement in a conscious patient. Nosotros present a case of a Locked-in Syndrome patient who received advice training with augmentative and alternative communication equipment past using eye blinks. After 3 weeks of grooming, the patient was able to make an effort to interact with other people, and associate a new give-and-take past Korean alphabet selection. Augmentative and alternative communication equipment which uses centre blinks might be considered to be benign in improving the communication skills of locked-in syndrome patients.
INTRODUCTION
Locked-in Syndrome (LIS) introduced by Plum and Posner in 1966, represents a astringent pontine infarction syndrome in which quadriplegia, lower cranial nervus paralysis and mutism are caused by vertebral and basilar artery thromboses. The LIS is a status in which functions of consciousness and cognition are maintained only there are defects of all movements other than eye blinks and vertical eye movements.1
The LIS patient's possible voluntary movements are eye blinks and vertical eye movements; hence, these functions play a office every bit a means of communication with the surrounding environment.
The recent evolution of assistive technology has invited patients who cannot conduct verbal advice to widen the options of augmentative and alternative communication (AAC), whereby each of these patients can effort to satisfy his/her demands. Farther, the distribution of computers has been expanded and internet access has become easier. Therefore, various attempts have been made for the communication of patients who cannot comport out any physical activities.
Nevertheless, no research has been conducted on LIS patients' communication in Korea. Therefore, this research discusses the preparation of communication using AAC, together with a review of related literature.
Instance REPORT
In our hospital, a 52-year-former male patient was hospitalized who had paralyses of the upper and lower limbs, mutism, respiratory disorder, and dysphasia. The patient had entered a Korean oriental medical clinic with dizziness and dysarthria 5 months prior to the hospitalization. He showed a sudden progress of altered mental status, quadriplegia, for 3 days. Due to these symptoms, he was transferred to the ER at a general infirmary. While hospitalized in the general infirmary, in tests using Magnetic Resonance Imaging (MRI) scan and angiographical inspection he was diagnosed with infarctions of cerebella, pons, midbrain, corpus callsum, of the left occipital lobe and the right thalamus caused by bilateral vertebral and basilar avenue occlusions. At ICU, he received astute stage treatments (due east.g. tracheostomy and respirator, anticoagulation therapy, etc.). After these treatments, he was in a stable status, receiving hospital treatments for approximately 4 months. In social club to receive comprehensive rehabilitation therapy, he entered our hospital approximately 5 months later on later on he showed the previously mentioned symptoms. When showing these symptoms 5 years agone, he was diagnosed with diabetes and high blood pressure and he was then administered drugs continuously. He had no particular family history of these diseases.
Later on he was admitted into our infirmary, he received a neurological exam. The test showed that he was in a conscious state. However, his cognitive and perceptual abilities could not be determined due to the difficulty in communicating with him. The cranial nervus examination showed a voluntary minute tilt of the right side of his head. He could move his eyeballs in limited perpendicular and horizontal directions and blink his eyes. Besides, bilateral facial paralyses were observed. He could not project his voice nor could he consume anything. He could not move his tongue and the gag reflex did non occur.
The muscular strength of the upper and lower limbs measured by Manual Muscle Testing (MMT) is grade nothing. The spinal reflex of the limbs increased. The muscle tone assessment showed that the right upper and lower limbs and the left limbs were in Steps ii and 3 respectively. The patient'south Korean modified Barthel index (One thousand-MBI) was Grade 0/Grade 100 because he needed the carer'southward absolute assistance when performing all physical activities and activities of daily life.
The patient did non brand an endeavor to express himself. Afterwards he entered our hospital, he was trained to express "Yeah" or "No" by using a certain number of middle blinks. At the Rehabilitation Center attached to our hospital, he received alternative communication training to limited himself more concretely and actively, past using a software program related to the culling input device.
We fitted glasses on the side of his left centre by attaching these glasses to SCATIR (Self-Calibrating Auditory Tone Infrared) Switch (TASH, Roseville Usa), which detects an infrared reflection stimulated by physical activities considering he could not perform activities other than eye blinks (Fig. 1). Further, Switch Interface Pro5.0 (Don Johnston, Illinois, USA) was used, which delivers the input signal sent by the switch, operated when the patient blinks his eyes, to software programs and NeoSpeech Yumi (NextUp Technologies LLC, North Carolina, USA), a vox output software plan (Fig. 2).
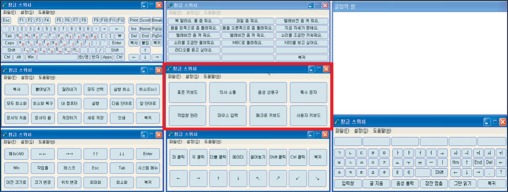
According to the situation, he received training in the position of sitting on a bed or a wheelchair 40 minutes a solar day for 3 weeks. During the kickoff week, the software programs Evaluware (Tobii Assistive Engineering, Massachusetts, USA), Northern Grid For Learning activity (Northern Grid, Tyne and Wear, Britain), and Sim tech single switch software for preschoolers (Don Johnston, Illinois, U.s.), etc., were used to better the accuracy and speed of center blinks, (Fig. 3). This would encourage the patient to correctly click at regular time intervals (Fig. 4). For 2 weeks after the first week, he received training in the utilise of Clickey2.0 (Seong-Pil Kim, Seoul, Korea), which enables the relevant person non only to use all functions of a keyboard but by clicking simply also to output the called expression (i.e. a target word or sentence automatically scanned after its input operation) into a vocalism (Fig. 5).
The three-calendar week training enabled the patient to express uncomplicated words (e.g. "bada (ocean)" and his name by the combination of words using functions of the keyboard. Further, it enabled him to deliver some of his ideas and feelings by outputting the selected sentences (eastward.g. "I love you," "When am I leaving the hospital?" etc.) into a voice with an sound glossary part.
DISCUSSION
According to the existing studies, the mortality of LIS patients is approximately 67%2 and the survival charge per unit of the patients who survived 5, x and 20 years is 83%, 83% and xl%, respectively.three The xix-month follow-up investigation of LIS patients' functional recovery showed that only 21% of patients were able to perform some activities of daily life and the other patients (79%) needed other peoples' absolute assist for living.4
LIS patients who survive with clear consciousness for a long time and whose functional activity recovery is difficult demand a communication method for living at dwelling house and in society. Therefore, various types of devices and methods accept already been introduced and used. In 2001, the application of AAC was attempted, which used the activities of thumbs, the mentum, the head, and shoulders of 17 LIS patients in Finland; of these, ix patients were finally able to use a computer for Internet access or for sending and receiving daily eastward-mails.5 In add-on, in research carried out in the The states in 2003, two LIS patients diagnosed 11 years prior to 2003 returned to their position (i.eastward. lawyer and mathematics teacher) by communicating with eye blinks and a mouse stick.4
LIS is classified into three categories co-ordinate to whether or not physical activities and advice tin can be performed. Classic LIS refers to the loss of physical activities other than vertical heart movements, as defined by Plum and Posner. Incomplete LIS represents a condition in which voluntary activeness functions except for vertical eye movements remain and total LIS refers to a condition in which the functions of all physical activities are lost and communication between the relevant patient and others is incommunicable.6
It was observed that the patient in this report had a voluntary infinitesimal right caput tilt. The patient could move his eyeballs perpendicularly and horizontally and blink his optics. Co-ordinate to the above nomenclature, he can exist classified equally an incomplete locked-in syndrome (LIS) patient. However, he showed an intermittent rotary nystagmus of the eyeballs; he could functionally use the blink of the eyes. Therefore, we attempted to communicate with him by using this behavior.
If the eyes are close to the glimmer switch due to the characteristic of the input device while that device is being operated, the sensor will respond perceptively to the weak glimmer of the eyes and the operator cannot correctly click the scanning object. It is important for the operator to fix the correct position by adjusting properly the distance between the switch and the eyes. For the patient, at first we attempted to click by attaching the switch to the fixing frame attached to the bed. Withal, we devised a way for the patient to wear the spectacles in which the switch is attached and so that the distance between the switch and the optics can be maintained and that the carer can attach it easily. The patient received grooming in clicking every three seconds five days after the location is set up; the preparation showed a lxx% average accuracy. The patient was able to click every two seconds, 5 days after the training. The last one calendar week's training included his actual apply of the device.
The problem with the training is that the use of the device is greatly influenced by a patient's will and physical condition on the actual day of training. The relevant patient consumed a great deal of fourth dimension because, in the method, a phoneme was input into the patient, in which the cursor is circulated every two seconds. The frequent expelling of Phlegm caused the problem of a fall in concentration and accurateness of the training. In addition, the patient received training in the seated position and in tilting postures with various angles considering the patient had difficulty in maintaining a suitable position due to strained cervical muscles during the training. Finally, the patient received training in the seated position of tilting the truncus back at approximately 15 degrees, maintaining the head in the forrad direction past attaching a Velcro strap to the caput balance of a wheelchair. This report will be able to farther contribute to the creation of training effects and to an increment in quality to compensate for the defect of the training position in society to maintain the optimum position by manufacturing a rest for supporting a torso or an inner made of polyurethane for fitting the body shape.
When completing the training, the patient said that he had difficulty in directly combining words by using phonemes merely useful vocal sentences were convenient due to their relatively like shooting fish in a barrel employ. Farther, he added that he wanted to use this system continuously for his communication in the future.
The interaction betwixt the patient and the surrounding environs including with other people is not only a human'south basic desire but also an of import cistron for improving the quality of life. We cannot completely supersede normal language or emotional advice with the organisation applied for the patient. All the same, this AAC can grade and express not only a patient'southward basic demands just also personal decision-making or deeper ideas. We can consider the render of a patient skilled in the system to his/her career.
In the field of rehabilitation, the actual utilize of assistive technology needs the interest of the whole rehabilitation team and its continuous efforts. Also, it requires the evolution of a program convenient to use as well as professional training. This case proved that the efforts of the relevant persons (i.e. the medical team, therapists, the inquiry squad, the patient and his family) and the drove of their opinions could make it possible to devise an AAC (i.e. a possible communication method which is depression-priced, user-friendly, and accurate that has not been suggested previously) past enabling the patient to install a free software program adult in Korea into his/her computer and to install only the switch and the fixing frame.
Therefore, this case study volition supply not only the possibility and opportunity of communication to LIS patients, but it will also contribute to the generalization of the advice device and its actual employ, for the relevant patients' return to their family and order.
References
1. Smith Eastward, Delargy 1000. Locked-in syndrome. BMJ. 2005; 330:406–409. PMID: 15718541.
![]()
2. Patterson JR, Grabois G. Locked-in syndrome: a review of 139 cases. Stroke. 1986; 17:758–764. PMID: 3738962.
![]()
3. Doble JE, Haig AJ, Anderson C, Katz R. Damage, activity, participation, life satisfaction and survival in persons with locked-in syndrome for over a decade: follow-upwards on a previously reported cohort. J Head Trauma Rehabil. 2003; xviii:435–444. PMID: 12973273.
4. Casanova Eastward, Lazzari RE, Latta Due south, Mazzucchi A. Locked-in syndrome: improvement in the prognosis after an early intensive multi-disciplinary rehabilitation. Arch Phys Med Rehabil. 2003; 84:862–867. PMID: 12808539.
five. Söderholm S, Meinander One thousand, Alaranta H. Augmentative and alternative advice methods in locked-in syndrome. J Rehabil Med. 2001; 33:235–239. PMID: 11585156.
six. Bauer Thou, Gerstenbrand F, Rumpl Due east. Varieties of the locked-in syndrome. J Neurol. 1979; 221:77–91. PMID: 92545.
![]()
Fig. 1
Self-Calibrating Auditory Tone Infrared switch.

Fig. 2
Raw signals from the sensor were amplified and transferred to the control sensor box. Then, the controller sent information to the personal computer by using a phototransistor that converted optical signals into electric signals. A light emitting diode and a beep audio would occur with one blink (click) of the sensor by the patient. At the aforementioned time, electrical signals were output past voice through the Switch Interface.
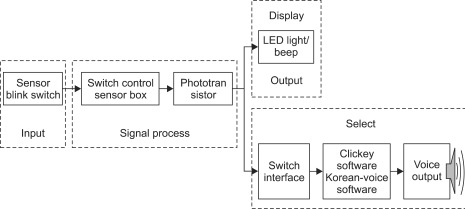
Fig. iii
Scanning training program for motor skills, response time and accuracy; (A) when patient clicks, the pointer moves to the target; (B) when patient clicks, bubble grows; (C) when entering into the squared circle, patients are required to click and; (D) when insects enter the circumvolve, patients are required to click.

Fig. four
The patient practicing preparation program using center blink.

Fig. 5
The Clicky2.0 automatically scans each item (alphabets, commonly used words and sentences) co-ordinate to the club and time interval previously set up. When a patient blinks his eye at the intended moment, a Self-Calibrating Auditory Tone Infrared switch is activated.
Source: https://synapse.koreamed.org/articles/1149520
0 Response to "2 Patterson Jr Grabois M Locked-in Syndrome a Review of 139 Cases Stroke 198617(4)758"
Post a Comment